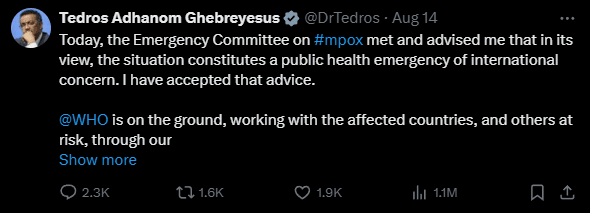
Mpox or formerly known as Monkeypox disease has been declared as a public health emergency of international concern by World Health Organization (WHO). On August 14th, the Emergency Committee on Mpox met with the director of WHO Tedros Adhanom Ghebreyesus on the topic. Later on, the present situation on Monkeypox disease has been declared as a public health emergency of international concern.
Following the decision, an article was published on the official UN website concerning the risks of this new mpox virus. In the past, the monkeypox disease was seen in some African countries, but it wasn’t deemed as threatening as the current Mpox. It is being said that the new strain of Mpox is far deadlier than the previous one.
Mpox current cases
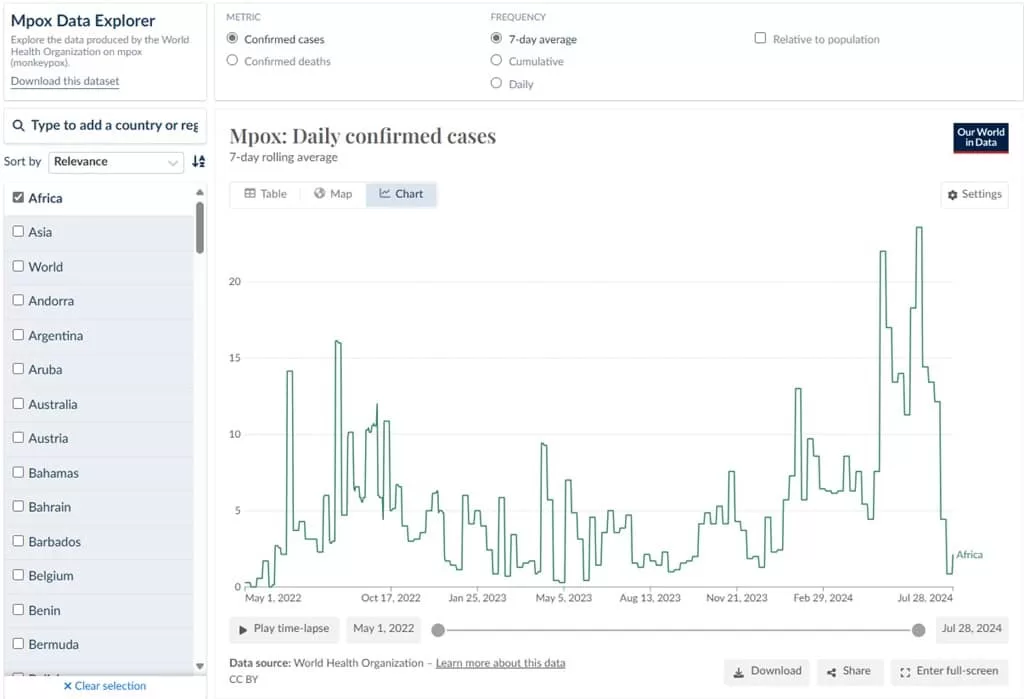
Mpox has been spreading in many countries in Africa particularly in Democratic Repulic of Congo (DRC) and its neighboring Burundi, Kenya, Rwanda, and Uganda. There is concern for the disease to spread beyond Africa. This year there were 14,000+ confirmed cases of the disease with 524 deaths, most of those being children. This is a significant increase comparing to the prior year.
Currently Mpox has spread to 13 countries in Africa and there are chances that it might spread too even more. “Stopping these outbreaks will require a tailored and comprehensive response, with communities at the centre, as always,” Dr. Tedros said.
What is the Mpox virus?
The disease is caused by viruses known as clades. At a meeting Dr. Tedros said that the clade 1b virus was seen in Democratic Repulic of Congo in the last year which spread “mainly through sexual networks”. The clade is reportedly much deadlier and have higher transmission capabilities. That is why it is spreading from person to person at a much faster rate.

While Clade 2 caused the global epidemic of 2022, which led to the declaration of an international public health emergency, Clade 1 had been active in the Democratic Republic of the Congo for many years.
According to Tedros, in the last month, almost 90 cases of successor clade 1b were reported in neighboring DRC counties that had not previously reported mpox cases.
Action taken by WHO to combat Mpox
In order to “understand and address the drivers of these outbreaks,” the WHO chief stated that the UN organization is collaborating with the governments of the impacted nations, the Africa CDC, and other partners.
For instance, he stated, “We are supporting laboratories to sequence viral samples and providing machines to analyze blood samples and confirm cases of mpox.” He went on to discuss training for healthcare professionals, “supporting case investigation and contact tracing” locally, and a host of other topics.
“In order to support surveillance, preparedness, and response activities, WHO has developed a regional response plan, requiring an initial $15 million,” Tedros stated. $1.45 million from the WHO Contingency Fund for Emergencies was used to finance this response.
In the upcoming days, more money will be made available, and the head of WHO is pleading with donors for additional funding.
What about Mpox vaccine
Mpox vaccination can help prevent the disease. There are currently two vaccines being used to stop the virus outbreak that have been licensed and recommended by the WHO.
Tedros also asked mpox vaccine producers to indicate interest in making the vaccinations under an Emergency Use Listing (EUL) call last week, with the goal of “accelerating vaccine access for lower-income countries which have not yet issued their own national regulatory approval.”

EUL will make it possible for partners like UNICEF to collect vaccines for distribution.
Tedros stated, “We are collaborating with all partners to enable fair access to diagnostics, immunizations, supplies for clinical care, and other tools.”
It is also important to note that there are no Mpox vaccine that is 100% effective. Cases were seen where people who received both vaccines got disease.
Precautions from WHO
The head of WHO published long-term guidelines for tracking mpox cases under the IHR in August of last year.
The deadline for these recommendations was August 20, 2024, but they will now be extended for a further year in order to “assist countries in responding to the chronic risk of mpox.”
Enhancing community protection through localized public health and social measures, offering resources and direction for clinical disease care delivery, and other suggestions are only a few of the suggestions.
In order to prevent transmission, treat those who are infected, and save lives, Tedros stated that WHO is “committed in the days and weeks ahead to coordinate the global response, working closely with each of the affected countries and leveraging our on-the-ground presence.”